Rayner ESCRS highlights – what surgeons are saying about their experience with Rayner IOLs
Posted on 3/11/2015
The 2015 meeting of the European Society of Cataract and Refractive Surgeons (ESCRS) held in Barcelona, Spain, featured a number of presentations describing surgeons’ experience with Rayner’s portfolio of lenses including the Sulcoflex, C-flex, M-flex and T-flex.
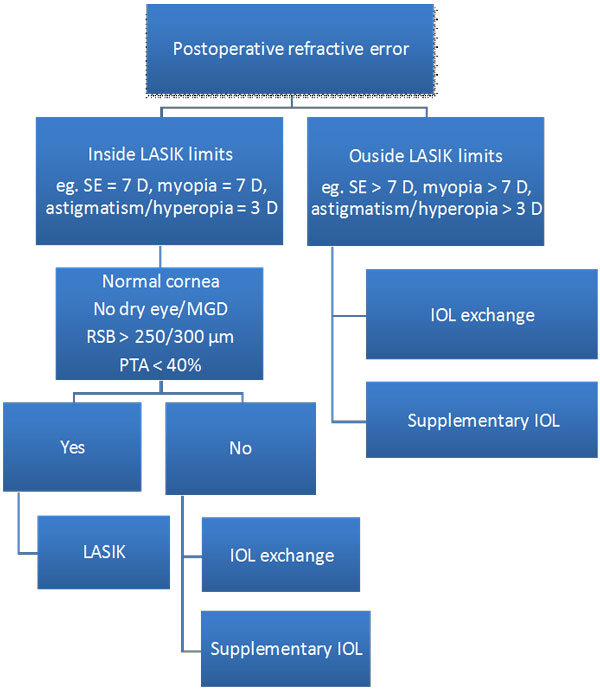
| The Sulcoflex Pseudophakic Supplementary IOL Supplementary IOLs Versus Wavefront-Guided LASIK for the Correction of Refractive ErrorsTiago Ferreira, MD Dr Ferreira described results from a comparative case series designed to compare visual outcomes in 33 eyes of 21 pseudophakic patients with residual refractive errors corrected either by implantation of a supplementary intraocular lens (IOL) (Sulcoflex Aspheric 653L or Sulcoflex Toric 653T, n=15) or wavefront-guided laser in situ keratomileusis (LASIK, n=18). Refractive target was emmetropia. At 12 months postoperative, mean UDVA (logMAR) was 0.08 ± 0.05 (Sulcoflex) and 0.06 ± 0.07 (LASIK) (p=0.544). Mean SE refraction was -0.28 ± 0.79 (Sulcoflex) and -0.33 ± 0.58 (LASIK) (p=0.830). Thirteen (87%) eyes in the Sulcoflex group and 17 (94%) eyes in the LASIK group were within ±1.00 D of emmetropia. Mean change in SE refraction from 1 week to 12 months postoperative was -0.04 ± 0.15D (Sulcoflex) and -0.25 ± 0.32 D (LASIK); p=0.004. Higher order aberrations (HOA) were similar between groups (HOA RMS 0.39 ± 0.18 [Sulcoflex], 0.29 ± 0.18 [LASIK]; p=0.234). There was no significant difference in contrast sensitivity (CS) except at 18 cd (better in the Sulcoflex group in both mesopic and photopic conditions, with and without glare; p=0.004). These data indicate that both surgical techniques provided excellent visual outcomes and refractive predictability. Stability of SE correction and CS at higher spatial frequencies (in both mesopic and photopic conditions with and without glare) were better in the Sulcoflex group. Based on these results, Dr Ferreira developed a decision tree for selecting one of the two techniques in pseudophakic patients (below).
. |
 |
|
The C-flexAspheric Monofocal IOL Ramin Khoramnia, MD (Germany) In an optical bench analysis, Dr Khoramnia and colleagues analyzed +26 D spherical C-flex 570C and aspheric C-flex 970C IOLs using the OptiSpheric (Trioptics, Germany) optical bench to evaluate the modulation transfer function (MTF) at 50 lp/mm and 100 lp/mm and the Strehl ratio using a 3 mm (photopic) and 4.5mm (mesopic) aperture. At 50 lp/mm, the MTF values were 0.713/0.806 (C-flex 570C/C-flex 970C) for a 3mm aperture and 0.297/0.594 for a 4.5 mm aperture. At 100 lp/mm, the MTF values were 0.527/0.634 for a 3mm and 0.198/0.345 for a 4.5 mm aperture. The Strehl ratio was 0.814/0.929 for a 3 mm and 0.236/0.487 for a 4.5 mm aperture. These data show that the aspheric IOL design achieved higher MTF values at both apertures. Moreover, the differences between the aspheric and spherical design were more pronounced at mesopic conditions. This suggests that patients with larger pupil sizes and/or working in mesopic conditions might benefit more from an IOL with an aspheric design. . |
 |
|
Incidence of Dysphotopsia Ashokkumar Vyas, FCRS (UK) In a single-centre, consecutive study, 40 patients without co-morbidity (average age, 76.6 years) underwent phacoemulsification surgery followed by implantation of the C-flex (570C) monofocal IOL through a 2.8mm incision. The incidence of dysphotopsia was assessed by a slit-lamp examination at one week, one month and three months postoperative. Patients were also asked to complete a questionnaire describing any symptoms at three months postoperative. Eighteen (45%) patients reported no ocular symptoms at their one or three month postoperative visit, and none of the 22 (55%) patients who did report visual disturbances found their symptoms debilitating. The most common post-operative visual phenomenon was glare, reported by 23 % of patients. Unwanted imagery was noted in 7 (17%) patients but was thought to be related to the lens in only one patient (2.7%). Almost all patients (98%) stated that they were either very satisfied or satisfied with their visual outcomes following C-flex lens implantation. A comparison of findings with those from a previous study which used the same questionnaire to assess dysphotopsia showed that incidence of unwanted imagery was lower with the C-flex than with the AcrySof single and three piece IOLs. Dr Vyas proposed that this may be due to the low refractive index (1.46) of the C-flex compared to hydrophobic lenses, and the lens design. . |
 |
|
Mixing and Matching Refractive Hydrophilic Acrylic Multifocal IOLs In a 2-year prospective study, 25 eyes of 21 patients with cataract and no other ocular pathology were implanted with the M-flex (630F) IOL. Four patients had bilateral multifocal implantation, seven patients had a multifocal IOL in one eye and a monofocal IOL in the other eye, nine patients were phakic in the other eye with varying degrees of lenticular changes, and one patient had no vision in the other eye. Findings showed that there was a statistically significant improvement in mean best corrected visual acuity (BCVA) and mean uncorrected visual acuity (UCVA) from preoperative at all follow-up visits up to two years. All the IOLs remained excellently centered and there were no intraoperative complications or explantations. Posterior capsule opacification (PCO) occurred in six patients, all of whom were successfully treated with YAG laser. Three patients complained of persistent glare and difficulty in night driving postoperatively. However, these visual symptoms dissipated over time as the patient adapted to the new lens and by six months postoperative, the problems had resolved. Spectacle independence was highest (100%) in the bilateral multifocal IOL group and lowest (66%) in the unilateral multifocal IOL only group.
Dr Mazhry concluded that mixing and matching with the M-flex is possible in motivated well-counselled patients and that multifocal IOL implantation in both eyes leads to optimal visual outcomes. |
 |
|
Long-Term Functional Results and Patient Satisfaction Dr Mrukwa-Kominek shared findings from a study designed to evaluate functional results and degree of patient satisfaction of different near additions of the M-flex 630F. Cataract patients received bilateral +3.00 D IOLs (Group I, 17 patients/ 34 eyes) or +4.00 D IOLs (Group II, 18 patients/ 36 eyes). At 48 months postoperative, the average UDVA in both groups improved significantly (p<0.001); 93% of eyes in Group I and 100% of eyes in Group II gained at least one row of vision (Snellen). There was also a significant increase in contrast sensitivity (p<0.001) in both groups for all spatial frequencies (3, 6, 12 and 18 cpd). While a significant increase in the average level of spectacle independence was noted in both groups (p<0.001), the overall increase in satisfaction in visual outcomes was greater in Group II (+4.00 D). No intraoperative complications were reported in either group. Overall these findings suggest that implantation of both models of the M-flex 630F was safe, stable, and effectively reduced dependence on spectacle correction.
|
 |
|
The T–flex Aspheric Toric IOLs LRIs Versus the T-flex IOL in the Correction of Astigmatism Mayank Nanavaty, MBBS, DO, FRCOphth In a prospective, randomized controlled study that compared subjective and objective outcomes after LRIs versus toric IOL (T-flex) implantation for the correction of astigmatism (0.75 D to 2.5 D), the first eye of 80 patients was randomized to receive either LRI (40 patients) or the T-flex IOL (40 patients). Between the two groups, at all follow up visits (1, 3 and 6 months), there was no significant difference in LogMAR UDVA, BCDVA, uncorrected near visual acuity (UCNVA), and best corrected near visual acuity (BCNVA). Although the mean refractive cylinder and SE were lower with toric IOLs than with LRIs, it was not significantly different. The LRI group had larger change in mean refractive astigmatism, but again, it was not statistically significant. Keratometric astigmatism was significantly less in the LRI group at all follow up visits, but there was no difference in mean keratometry between groups. Findings also showed that difference in pre and postoperative spectacle independence was 12.7% greater in T-flex group. Mr Nanavaty also noted that there was no significant rotation of the T-flex.
|
 |
|
Outcomes After Correction of High Astigmatism Dr Su Ling Young presented findings from a three-month prospective study in which 66 eyes with a high degree of corneal astigmatism (range, +2.5 D – +6.5 D) were implanted with the T-flex IOL. The results showed that postoperatively, 11% of patients achieved an uncorrected distance visual acuity (UDVA) of 6/6 or better, 32% reached 6/9 or better and 90.9% achieved 6/12 or better. Best corrected distance visual acuity (BCDVA) was 6/6 or better in 53% of patients and 6/12 or better in 98.4% of patients. The mean residual astigmatism was 1.10 D +/- 0.88 D, and <1 D in 66% of patients. A vector analysis showed an overall reduction in refractive astigmatism of 3.87+/- 1.46 D. Findings also showed that T-flex had excellent rotational stability; 92.4% (61 eyes) had rotation of <10° and only 2 eyes (3.03%) required postoperative IOL rotation.
Overall, these results concur with other results published showing the reliability of T-flex across countries and surgeons and indicate that the T-flex is effective in correcting high levels of corneal astigmatism.
|
|
|
Rotational Stability and Visual Outcomes Visual quality, astigmatism reduction and rotational stability of the T-flex IOL were assessed in a prospective study of 44 eyes (29 patients). Patients were divided into three groups – Group 1 targeting emmetropia, Group 2 targeting myopia (-2.0 D) and Group 3, which included eyes with amblyopia. Three months following implantation of the T-flex(mean spherical power, +19.37 [range +7.0D to +30.0D]; mean cylinder, +2.40 [range +1.0 to +8.5]), 54% of patients in Group 1 had a mean UDVA (LogMAR) of 0.00; 77% achieved 0.05 or better, 95% reached 0.10 or better, and 100% achieved 0.20 or better. In Group 2, mean corrected distance visual acuity (CDVA, LogMAR) improved from 0.16 preoperatively to 0.06 postoperatively, mean astigmatism reduced from 2.41 D to 0.75 D, and mean refractive sphere reduced from -7.55D to -2.29 D. Improvements in UDVA, CDVA, refractive astigmatism and refractive sphere were also noted in Group 3: Group 3 Findings
Findings also showed that 94% of eyes had rotation of < 10° and 61% of eyes had rotation of < 5°; overall IOL rotation was 4.05°. These data demonstrate that the Rayner T-flex IOL is an effective and reliable option to correct corneal astigmatism in cataract and refractive surgery.
|
|
|
Comparison of Visual and QoL Outcomes from LRIs vs Toric IOL Implantation for Astigmatic Correction Dr Dimitry and colleagues presented findings from an ongoing prospective, randomized controlled study designed to compare post-operative visual outcomes (LogMAR) of UDVA, BCDVA and spherical equivalent (SE) in patients undergoing astigmatic correction during standard cataract surgery with limbal relaxing incisions (LRIs) or toric IOLs (tIOLs [T-flex]). Forty eyes with astigmatism (0.75 to 2.5 D) were recruited in each group. There was no significant difference in the one month mean post-operative UDVA and BCDVA between groups, nor were there any differences in near vision outcomes or refractive outcomes between groups. There was also no significant difference in the mean post-operative Quality of Life Impact of Refractive Correction scores between LRI and tIOL groups. However spectacle independence was reported to be 8.9% greater in the toric IOL group.
These data indicate that cataract surgery combined with astigmatic correction offered a similar improvement in visual outcomes in both the LRI and toric IOL groups. Astigmatic correction with LRIs or toric IOLs offers similar quality of life outcomes for astigmatism between 0.75 D and 2.5 D at one-month postoperatively. |
|





